That the health delivery system is in a crisis is no longer news. Governments, since the mid 1970s have battled with this crisis with very little success to show. We have had some very good ministers of health such as the late Colonel Serlomey and Nuamah Donkor Esq. attempting to fix the debilitating problems of health care without success. The enhanced construction of new hospitals supported by donor funding across the country from the ultra modern regional hospitals to new district hospitals seem not to have had any impact on the health delivery crisis.
I was admitted to the Medical and Surgical Emergency of the Korle Bu Teaching Hospital on Monday December 1, after my attempts to treat what I thought was malaria proved futile. As is usual with majority of the population, the frequency of malaria occurrence has reduced its impact in our psyche to a common ailment along the lines of a mild headache leading to a situation where the first place of call for relief is the pharmacy shop rather than the hospital/clinic. Little did I know that hiding behind the malaria symptoms were other conditions including gastric ulcer, anaemia, diabetes, jaundice etc? I felt so stupid not reporting to a health facility before attempting self-medication anytime I had to explain my situation to the medical team that looked after me.
The essence of this write up is not about me but about the health delivery system. When my driver finally delivered me to the Medical and Surgical Emergency on December 1, 2003, the place was jammed with suffering humanity in one stage of pain or the other. The medical team on duty was stretched to their limit with an overflow of patients in a very confined space. The corridor was choked with patients of both sexes. People were receiving their transfusion on benches and trolleys in the corridor in the unbearable heat of the medical reception. There seem to be even more doctors at the emergency than nurses; attesting to the depletion of nurses in the medical delivery system. With a referral note appropriately signed, it took me between three to four hours before receiving attention. In between, my assistant had tried retrieving the referral note from the nurse at the reception. He had wanted to send me to the Trust Hospital after seeing me writhing in pain on the bare floor. I could neither sit on the hard bench nor stand and therefore was lying on the bare and probably infected floor.
Finally, a bed became available. From that point, I received the best care and attention available in the circumstances. As a friend was to later remark, the title might also have come in handy. However, within fifteen minutes of my being assigned a bed the first infusion being administered, the patient to my left passed away without any screening or privacy. When the young doctor pronounced to the team ‘I am afraid we have lost him’, my heart sunk. Within another hour, the patient to my right also passed away! I had the fright of my life and my religious part took over my being. Facing the reality of death this way has a sobering effect and needless to say, it enhanced my prayer life! I was transferred to the more private inner ward of the Medical and Surgical Emergency facility later that night. After a few days, here I was again transferred to Medical Ward 4L. The ward is located in a temporal structure. The main medical ward had been evacuated for the last four years or so due to the poor state of disrepair of the facility. There are finally signs of activity on the old bloc but only heaven knows how long it would be under rehabilitation. Meanwhile, the present accommodation is highly unsuitable and compressed to meet the standards expected of the nation’s premier teaching hospital.
My admission forced me to confront the reality of health care provision seriously for the first time in recent years. As a management professional (both development and business) I had neglected this area for quite a while. Thinking through the health care delivery, a number of issues stand out:
Human Resource Development and Management
The crisis of delivery begins at the doorstep of human resource development, management and retention. The shortage of skilled medical personnel, occasioned largely in the case of nurses and doctors, by an unprecedented exodus to Europe and North America is reached dangerous levels. Medical and nursing cover, even at Korle Bu is so thinly spread that we should be thinking of employing occupational psychologists to counsel our doctors and nurses. They are simply overworked and stressed out. In this state, the possibility of mistakes of judgement is magnified. At the Medical and Surgical Emergency, there were times, particularly at night when there were more doctors on duty than nurses! Our nurses seemed to have fled the country faster than ever the doctors. You are now more likely to find nursing officers and very junior nurses (including student nurses) manning the wards and other facilities. The experienced staff and senior staff nurses now seem to be an endangered species in our hospitals.In the emergency ward, patients on admission are expected to have relatives staying with them at night to attend to them since there are not enough nurses and ward assistants (now called health assistants) to provide nursing care. When you therefore go on admission, another member of the family is more or less jointly admitted! And yet, here we are talking about productivity. You need to see the rush into the wards early morning by family members to feed, bathe and dress patients before ward rounds to appreciate the seriousness of the situation. As a nation, we need to get our priorities right. The demoralised staff we have manning the Ghana Health Service cannot deliver the foundation needed for sustained economic growth until there is a radical reappraisal of roles and benefits. If the establishment quota for Korle Bu is two thousand nurses and we have five hundred, what stops us from dividing the remuneration of say a thousand five hundred over the five hundred at post and paying them well? The argument that other professionals would complain is neither here nor there. If we have a shortage of a particular skill, let’s use the market to fill that gap. If we started paying our nurses and doctors well, the drain would reduce radically. If three people are doing ten people’s work, let’s at least pay them eight people’s salaries. And as a junior doctor put it, ‘. even to access our small ADH, we have to go on strike before …’.
Are those in charge of human resource development reacting appropriately to the crisis we have on our hands? Are we being innovative or we are still soaked in yesterday’s practices? While on my sick bed, I was thinking of how we can increase the number of nurses in the system radically without sacrificing quality. A look at the training programme for registered nurses is necessary here. Student nurses spend three years in the various Nurses Training Colleges in the country. They then do a year’s rotation before being registered the Nurses and Midwifery Council. In 1953 when the internal self-government of Kwame Nkrumah launched the accelerated education policy, the need arose for thousands of teachers to meet demands of new basic schools. The innovative way out was to introduce the Teacher’s Certificate B programme where instead of the normal four years at Teacher Training College, students did two years and were awarded a certificate B. After coming out to teach for a number of years, these teachers went back to college and did another two years for the award of certificate A. The number of teachers coming out of the training colleges was thus double by this innovation. Both the Ghana Health Service and the Ministry of Health can learn from this. What stops our student nurses from doing a one year programme divorce of ward duties (practical) in their first year and coming out to do two years of ward nursing before going back for another year to complete their formal training? While on the two-year ward duty, they should be paid the salary of an enrolled nurse instead of their student allowances. By this way, we would increase the number of nurses in our hospitals and our clinics without compromising quality.
Funding and resource allocation
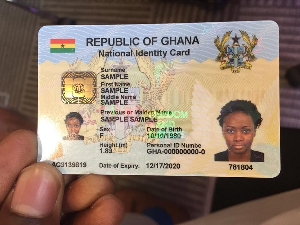
The funding of health care delivery and its ancillary services has often been contentious in the best of times. What level of state funding is adequate to meet the cost of health care provision? And should the whole cost be borne by the state through taxation? Is there a role for private sector participation in both the funding and delivery of health care? What proportion of common resources should be devoted to health care provision and delivery? Governments in the past have tried a number of methods to pay for health care delivery without success. We have had times in the past where the state underwrote all but the minimum costs. We have also had the much-criticized cash and carry interspersed with sprinklings of private and community insurance schemes. Currently, government policy is the introduction of a national health insurance scheme to pay for health care delivery. This is potentially a better solution than the cash and carry in all its various permutations. However, there is the real danger of this suffering the fate of the educational reform programme that gave birth to the Junior and Senior Secondary School concepts. The number of civil society groups that have called for a further examination of the health insurance law is very well widespread. And yet, our political masters, seeming to work towards some unknown time frame would not countenance this ‘delay’ thus steam rolling the bill through a docile parliament. Issues of transferability, identification, universality etc. have been jettisoned on the alter of expediency.In any case, what levels of premiums are going to be adequate to meet the ever-increasing cost of delivery? If one CT Abdominal scan cost one million two hundred thousand cedis at Korle Bu Teaching Hospital, what level of premiums would be needed to be able to provide such high tech services? And yet, we all agree that health service must be properly resourced. In a poverty prime society, the common purse and by that taxation provides the best guarantee of adequate funding for the health services. Three possible approaches come immediately to mind. An increase in VAT to be ring fenced to funding health, a specific tax on income tax for health or a tax on petroleum products specifically for health. VAT has unfortunately become a taboo topic because of the shortsighted position taken by the governing party while in opposition. The net for income tax unfortunately still misses more income earners than it ropes in. The most realistic of the three is therefore a tax on all petroleum products for the specific purpose of funding health care. This would ‘catch’ every resident either directly or indirectly. In any case road accidents are increasingly putting a strain on the meagre resources available. A five hundred cedi health tax on a litre fuel and lubricants as well as on a kilo of LPG would bring in billions of cedis a month to be used to fund a reasonable level of health delivery. The national health insurance premium can then be kept at an affordable level to rope in as many Ghanaians as possible while developing the appropriate structures for the entrenchment of the concept.
I would advocate that a very independent board be established by an Act of Parliament to administer the Health Fund so created from petroleum tax. The lessons of the GETFund should be learnt so that no government can divert manoeuvre the use of the Fund. The current accusation and counter accusation on the use of the GETFund can serve to fashion a more acceptable structure for administering the Health Fund. A percentage of this fund must be set aside for maintenance of existing infrastructure and training. I would suggest that the fund should not be used to put up new facilities - that should continue to be the burden of budgetary allocation from central government. Ghanaian governments have never been weak in sourcing funds to put up new hospitals, health centres and clinics. For whatever reason, they have always excelled in that regard. However, the same cannot be said of maintenance.
The Teaching Hospitals and the Ghana Health Service should also be re-oriented to seek value for money in the way they expend funds. Departments and Units should as much as possible become cost centres to monitor the use of funds and to also generate funds. This leads to the management of both the Ghana Health Service and the various hospitals.
Management Structure and Mindset
It still surprises me that medical specialists man our hospitals either as chief executives and medical superintendents. This is absurd in a country where shortage of specialists is the norm rather than the exception. In Europe and North America, where health delivery systems work, non-medical management specialists run hospitals while medical specialists run their departments and clinics. We should have the courage to appoint non-medical specialists to manage our hospitals in the best traditions of modern management. We need to train our hospital administrators to very high degrees of competence to take over the running of these hospitals. The recognition that management is a speciality seems to have escaped the Ministry of Health in Ghana. Medical practitioners must remain medical practitioners. The number of experienced doctors manning civil service type positions in the Ministry of Health, Ghana Health Service and the District Health establishments is indicative of the convoluted logic that dominates the mindsets of policy makers. We should start working towards running hospitals as Trusts with their own boards of governors. The make up of the boards should also ensure some local representation. The Ghana Health Service should be more of a coordinating body for these Trusts setting broad implementation guidelines from the policy directives of the Ministry of Health. All personnel of the various hospitals, other than the Teaching Hospitals should be employees of the Ghana Health Service on secondment to the various Trust Hospitals. Once the Ghana Health Service is not directly involved in the running of these hospitals, it would then be in a better position to supervise these Trusts and insists on the maintenance of acceptable standards of care. Another key function of the Ghana Health Service would be the provision of training facilities including specialists training for both medical and non-medical staff of the Trust Hospitals.
National Policy
At the core of the health delivery crisis is an incoherent and inconsistent national policy or lack of it on health. What is our blue print on health care provision? If such a blue print exists, how well known has its contents been communicated to the broad masses? And what is the priority placed on health care delivery? As a leading doctor intimated during my stay at Korle Bu, the largest single killer in Ghana is poverty. If we are desirous of developing a robust economy ready to face the challenges of this century and beyond, then health and education should take the pride of place in our worldview.What is the policy on malaria control for example? Are we doing anything to tackle the disease from the root point of sanitation? Are the necessary linkages been drawn and dealt with? What is the cost of ill health to the economy in a given year? Health care should be seen in a systems methodology rather than just as a medical intervention. A systems view would link prevention to health delivery. It would also link good health to economic performance thereby justifying the provision of adequate resources to health care provision and delivery. Productivity would continue to be low as long as health care is marginalized. The number of non health care professionals forced to physically care for patients in hospitals is mind boggling and a definite drain on productivity.
Lets have an internally consistent and coherent health policy debate with no sacred cows. The Ministry of Health should be at the forefront of this debate as well as education. Why should the health budget not receive the priority it deserves? How can we be serious when patients have to go to the Cocoa Clinic for endoscopy because the machines at Korle Bu are broken down? Lets sit up as a nation and tackle our health care needs with urgency. We should not let poverty sentence our people to premature deaths. This must stop through collective national action.