Alyssa Tapley, 16, bin tink say she go die of leukaemia bifor e receive di treatment
Alyssa Tapley, 16, bin tink say she go die of leukaemia bifor e receive di treatment
One therapy wey pipo bin once reason as achievement for science fiction don reverse aggressive and incurable blood cancers for some patients, doctors report.
Di treatment process involve make dem perfectly edit di DNA for white blood cells and transform dem into cancer-fighting "living drug".
Di first girl to receive dis kain treatment wey BBC report her tori for 2022 still dey free of di free of di disease and now dey plan to bicom cancer scientist.
Now, dem don treat eight more children and two adults wey get T-cell acute lymphoblastic leukaemia, wit almost two thirds (64%) of patients in remission.
T-cells suppose be di body guardians – dia work na to find and destroy threats - but for dis form of leukaemia, dem dey grow out of control.
For those wey dey di trial, chemotherapy and bone marrow transplants wey dem do fail. Apart from di experimental medicine, di only option wey remain for dem na to make dia death more comfortable.
"I bin really tink say I go die and I no go grow up to do all di tins wey evri pikin deserve to fit do," 16-year-old Alyssa Tapley from Leicester tok.
She be di first pesin for di world to receive di treatment from Great Ormond Street Hospital and now she dey enjoy life.
Di revolutionary treatment wey she receive three years ago bin involve make dem remove her old immune system and grow a new one.
She spend four months for hospital and she no fit see her brother, sake of fear say e fit bring infection.
But now her cancer dey undetectable and she only need annual check-ups.
Alyssa dey do her A-levels, di Duke of Edinburgh Award, she dey eye driving lessons and dey plan her future.
"I wan do apprenticeship for biomedical science, and hopefully one day I go study blood cancer research too" she tok.
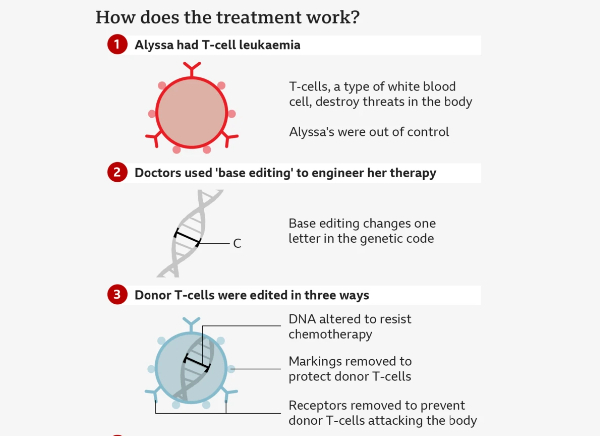
Di team for University College London (UCL) and Great Ormond Street Hospital bin use one technology dem call base editing.
Bases na di language of life. Di four types of base for DNA - adenine (A), cytosine (C), guanine (G) and thymine (T) – na di building blocks of our genetic code.
Just as letters for di alphabet dey spell out words wey carry meaning, di billions of bases for our DNA dey spell out di instruction manual for our body.
Base editing dey allow scientists to zoom to one precise part of di genetic code and den change di molecular structure of just one base, dem go convert am from one type to anoda and rewrite di instruction manual.
Researchers bin wan use di natural power of healthy T-cells to find out and destroy threats and turn dat against di T-cell acute lymphoblastic leukaemia.
Dis na tricky feat. Dem get to engineer di good T-cells to hunt di bad ones without di treatment destroying itself.
Dem start wit healthy T-cells from one donor and start to dey modify dem.
Di first base edit disable di T-cells target mechanism so dem no got fit attack di patient body.
Di second edit dey remove one chemical marking wey dem call CD7. E dey on all T-cells. To remove am dey essential to prevent di therapy from self-destructing
Di third edit na "invisibility cloak" wey no dey allow chemotherapy drug kill cells.
Di final stage of genetic modification dey instruct di T-cells to go hunting for anything wey get CD7 marking on am.
Now di modified T-cells go destroy evri oda T-cell dem see weda dem dey cancerous or healthy, but dem no go attack each oda.
Dem dey infuse di therapy into patients and if dem no detect dia cancer afta four weeks, di patients go den get a bone marrow transplant to regrow dia immune system.
"A few years ago, dis for be science fiction," Prof Waseem Qasim from UCL and Great Ormond Street tok.
"We get to basically dismantle di entire immune system.
"Na deep, intensive treatment, e dey very demanding on di patients, but wen e work, e dey work very well."
Di study, wey dem publish for di New England Journal of Medicine, don report di results of di first 11 patients treated across Great Ormond Street and King's College Hospital.
E show say nine pipo achieve deep remission wey allow dem go for a bone marrow transplant.
Seven still dey disease-free between three months and three years afta treatment.
One of di biggest risks of treatment include infections wen di immune system still dey wiped out.
In two cases, di cancer lose dia CD7 markings, e make am hide from di treatment and e return for di body.
"Given how aggressive dis particular form of leukaemia be, dis na quite striking clinical results, and obviously, I dey very happy say we don manage to offer hope to patients wey otherwise don lose hope," Dr Robert Chiesa from di bone-marrow transplant department for Great Ormond Street Hospital tok.
Dr Deborah Yallop, consultant Haematologist for King's, tok say: "We don see impressive responses in clearing leukaemia wey seem incurable – e be very powerful approach."
Commenting on di research, Dr Tania Dexter, senior medical officer for UK stem cell charity Anthony Nolan, say: "Considering say dis patients get low chance of survival bifor di trial, dis results bring hope say treatments like dis go continue to advance and become available to more patients."

Alyssa now dey enjoy life