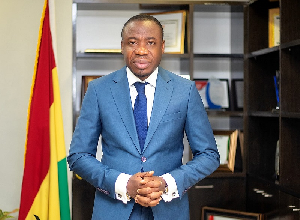
 Dr Da-Costa Aboagye is the NHIA CEO
Dr Da-Costa Aboagye is the NHIA CEO
The Private Health Facilities Association of Ghana (PHFAoG) has commended the Chief Executive of the National Health Insurance Authority (NHIA), Dr. Da-costa Aboagye, and his team for their unwavering commitment towards prompt payment of claims.
Describing recent payments by the NHIA as unprecedented, the Association said the drive has brought great relief to service providers under the National Health Insurance Scheme.
The commendation was contained in a communique issued after the Association's 4th Annual General Conference, held from September 18th to 20th, 2024 and signed by its President, Dr Kwame Buabeng Frimpong.
"PHFAoG acknowledges the Authority’s extraordinary efforts in releasing a significant amount of funds to settle claims owed to healthcare service providers across the nation.
“This timely intervention by Dr. Aboagye’s team has restored a level of financial stability, which is essential for sustaining quality healthcare delivery.
“The Authority has in the past weeks historically released a colossal amount for the payment of claims to service providers nationwide.
“Unfortunately, same cannot be said of some Private Health Insurance Schemes which have held to ransom, several months of unpaid claims due to service providers creating a financial bottleneck that threatens the sustainability of the services provided by their members,” the Association said.
The Association's commendation comes at a time when the NHIA has made considerable strides in addressing long-standing concerns regarding the delays in the payment of claims, a critical issue that had previously placed significant financial strain on healthcare facilities, particularly private ones.
In the last three weeks, the NHIA has released and disbursed over GH¢800 million for the payment submitted and vetted claims for April to July, 2024.
On August 17, 2024, the NHIA released GH¢151 million to cover claims from March 2024 for higher-tier healthcare providers and from April 2024 for lower-tier facilities.
This was preceded by a GH¢135.6 million payment in July, which settled claims up to February 2024 for higher-tier providers and up to March 2024 for lower-tier facilities.
On April 30, 2024, the NHIA released GHS170,775,035.07 to cover predominantly claims of January and February 2024 for lower-tier facilities, who form the majority of healthcare providers, and up to November 2023 for upper-tier facilities and healthcare providers.
On March 22, 2024, the NHIA paid GH¢180 million to various categories of healthcare providers across the country for claims submitted and vetted up to December 2023.
On February 13, 2024, the NHIA paid GHS130,244,000.00 to 4,850 Mission, Public, Private, and Quasi-Public healthcare providers nationwide largely for claims submitted for the month of October 2023.
Appeal for Expedited Tariff Review
In addition to commending the NHIA for its role in claims payment, PHFAoG has also urged the Authority to expedite the ongoing review of tariffs for healthcare services, a matter of great concern to private health facilities.
The Association noted that it had been part of the review committee working alongside the NHIA to ensure that the revised tariffs reflect the current economic realities faced by healthcare providers.
Despite their contributions to the review process, PHFAoG expressed apprehension regarding the adequacy of the upcoming tariffs, fearing they may not align with the current pricing dynamics in the healthcare market.
"Our primary concern is whether the new tariffs will accurately reflect the market conditions to the extent of eliminating illegal charges or payments known as co-payment under the NHIS, which have become a source of frustration for both service providers and the National Health Insurance Scheme (NHIS).
" Co-payment, a situation where patients are required to pay additional fees beyond what is covered by the NHIS has become increasingly common due to the perceived inadequacy of existing tariffs.
To address this issue, the Association has called on the NHIA to reconsider its approach to benchmarking tariffs against inflation rates, pointing out that inflation does not necessarily reflect the pricing of medical commodities.
"Pricing of healthcare inputs is based on market forces, not inflation," the statement read.
Re-call
However, while addressing the conference in Koforidua, Dr Aboagye assured all service providers under the NHIS that the Authority is pursuing pragmatic reforms to Scheme, which will help address their concerns.
He mentioned components of the reforms to include prompt payments of vetted claims to ensure payments were current; automatic price adjustment to regulate pharmaceutical pricing; E-pharmacy policy to enhance medication accessibility under the scheme and the collaboration with the National Identification Authority to provide Ghana cards for 6.3 million young people between 6 and 14 to enable them be captured unto the NHIS.
"While we have reviewed tariffs multiple times in recent years, pricing remain an anchor for both public and private facilities to charge illegal fees. For this reason, in this regime, our approach is let's do it well, that is why it has kept long.
“We have invited all stakeholders, development partners, everybody that matters to the table, trying to make sure that we get it right. This is why the process has delayed.
“Our goal is to introduce an automatic price adjustment mechanism that will help stabilise prices, especially in the pharmaceutical sector,” Dr Aboagye explained.